Journal Description
Antibiotics
Antibiotics
is an international, peer-reviewed, open access journal on all aspects of antibiotics, published monthly online by MDPI. The Croatian Pharmacological Society (CPS) is affiliated with Antibiotics and its members receive discounts on the article processing charges.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, SCIE (Web of Science), PubMed, PMC, Embase, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q1 (Pharmacology and Pharmacy) / CiteScore - Q1 (General Pharmacology, Toxicology and Pharmaceutics )
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 15.8 days after submission; acceptance to publication is undertaken in 2.5 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
4.3 (2023);
5-Year Impact Factor:
4.6 (2023)
Latest Articles
Antibiotic Considerations in the Treatment of Maternal Sepsis
Antibiotics 2025, 14(4), 387; https://doi.org/10.3390/antibiotics14040387 (registering DOI) - 7 Apr 2025
Abstract
Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, remains the third leading cause of maternal mortality globally. Pregnancy-associated physiological adaptations predispose pregnant individuals to infection, impair maternal response to infection, affect antibiotic pharmacokinetics and metabolism, and complicate diagnosing
[...] Read more.
Sepsis, a life-threatening organ dysfunction caused by a dysregulated host response to infection, remains the third leading cause of maternal mortality globally. Pregnancy-associated physiological adaptations predispose pregnant individuals to infection, impair maternal response to infection, affect antibiotic pharmacokinetics and metabolism, and complicate diagnosing infections and sepsis. Therefore, it is tantamount that clinicians readily recognize maternal sepsis and understand antibiotic regimens and treatment principles to avoid adverse maternal outcomes. In this article, we present an overview of the diagnosis and management of maternal sepsis and the physiological changes in pregnancy that alter antibiotic pharmacokinetics. Common microorganisms implicated in maternal sepsis are discussed with an emphasis on E. coli and Group A Streptococcus due to their prevalence and morbidity in the pregnant population. Lastly, we provide an overview of commonly used antibiotics and dosage recommendations in the treatment of maternal infection and sepsis.
Full article
(This article belongs to the Special Issue Sepsis Management and Antibiotic Therapy)
Open AccessArticle
Efficacy of Ceftobiprole and Daptomycin at Bone Concentrations Against Methicillin-Resistant Staphylococcus aureus Biofilm: Results of a Dynamic In Vitro PK/PD Model
by
Mikel Mancheño-Losa, María Ángeles Meléndez-Carmona, Carlos Lumbreras and Jaime Lora-Tamayo
Antibiotics 2025, 14(4), 386; https://doi.org/10.3390/antibiotics14040386 (registering DOI) - 5 Apr 2025
Abstract
Background: The presence of biofilms and low antimicrobial concentrations in bone tissue make prosthetic joint infections (PJI) difficult to treat. Ceftobiprole (CTO) has a potential role in MRSA PJI. This study evaluated the efficacy of ceftobiprole and daptomycin (DAP) alone and in
[...] Read more.
Background: The presence of biofilms and low antimicrobial concentrations in bone tissue make prosthetic joint infections (PJI) difficult to treat. Ceftobiprole (CTO) has a potential role in MRSA PJI. This study evaluated the efficacy of ceftobiprole and daptomycin (DAP) alone and in combination against MRSA biofilms at expected bone tissue concentrations. We assessed whether CTO-DAP outperformed DAP combined with a non-anti-MRSA beta-lactam (cefazolin [CZO]). Methods: A dynamic in vitro PK/PD biofilm model (CDC biofilm reactor) was used to simulate concentrations expected in cortical bone at a standard dosing of DAP (10 mg/kg/24 h), CTO (500 mg/8 h), and CZO (2 g/8 h), and assess performance against a 48-h MRSA biofilm from two clinical isolates that cause PJI (MRSA-1811 and MRSA-1733). Time–kill curves using the log change method (Δlog10 CFU/cm2) assessed antimicrobial efficacy over 56 h. Resistance emergence was monitored. Results: Although both monotherapies were active, neither reached bactericidal levels nor was one superior to the other (Δlog10 CFU/cm2 CTO vs. DAP: −1.44 ± 0.25 vs. −1.50 ± 0.01 [p = 0.686] and −1.55 ± 0.74 vs. −0.56 ± 0.36 [p = 0.108] for MRSA-1811 and MRSA-1733, respectively). Only in the MRSA-1811 isolate did the CTO-DAP combination improve the activity of each monotherapy, without achieving a synergistic effect (Δlog10 CFU/cm2: CTO-DAP −2.087 ± 0.048 vs. CTO −1.436 ± 0.249 [p = 0.013] and vs. DAP −1.503 ± 0.011 [p = 0.006]). No combination therapy (CTO-DAP vs. DAP-CZO) outperformed the other in either strain. No resistant bacterial subpopulations appeared with any antibiotic regimen. Conclusions: At clinically relevant concentrations, ceftobiprole and daptomycin showed similar activity against MRSA biofilms. The CTO-DAP combination showed comparable efficacy to DAP-CZO.
Full article
(This article belongs to the Special Issue Bone and Joint Infections: The Challenges of Prevention, Diagnosis and Treatment and Opportunities for Future Research)
►▼
Show Figures

Figure 1
Open AccessArticle
Structure–Activity Study of the Antimicrobial Lipopeptide Humimycin A and Screening Against Multidrug-Resistant Staphylococcus aureus
by
Md Ramim Tanver Rahman, Louis-David Guay, Ismail Fliss and Eric Biron
Antibiotics 2025, 14(4), 385; https://doi.org/10.3390/antibiotics14040385 (registering DOI) - 5 Apr 2025
Abstract
Background: The emergence of multidrug-resistant (MDR) Staphylococcus aureus presents a critical global health challenge due to treatment failures and high mortality rates. Faced with this growing threat, new antimicrobials with original modes of action are urgently needed, and antimicrobial peptides proved to be
[...] Read more.
Background: The emergence of multidrug-resistant (MDR) Staphylococcus aureus presents a critical global health challenge due to treatment failures and high mortality rates. Faced with this growing threat, new antimicrobials with original modes of action are urgently needed, and antimicrobial peptides proved to be promising alternatives. Objectives: The aim of this study is to explore the structure–function relationship of the lipopeptide humimycin A, compare the spectrum of activity of the synthetic analogs against a panel of S. aureus isolates, and investigate their binding to the humimycin target, the lipid II flippase MurJ. Methods: Humimycin A and 15 analogs were produced by solid-phase peptide synthesis, and their antimicrobial activity was evaluated by agar diffusion and microtitration assays against 19 S. aureus isolates from bovine mastitis and other pathogens. Results: Among the synthesized peptides, four humimycin analogs exhibited activity against methicillin-sensitive and methicillin-resistant S. aureus, as well as several isolates in the panel, including MDR S. aureus, with minimal inhibitory concentration values ranging from 0.5 to 256 µg/mL. Results from the structure–activity relationship study showed that the β-hydroxymyristoyl lipid chain and C-terminal carboxylic acid are essential for antimicrobial efficacy. In presence of human erythrocytes, the active humimycin analogs exhibited moderate hemolytic activity, suggesting selectivity indexes ranging from 3 to 27 against the more sensitive S. aureus strains. Critical micelle concentration measurements elucidated micelle formation and proved to not be essential for the antibacterial activity. Molecular docking and 100 ns simulations with the lipid II flippase MurJ (PDB: 5T77) provided favorable binding energy. Conclusions: The findings underscore the potential of humimycin analogs as antimicrobials for preventing and treating MDR S. aureus infections in veterinary, animal husbandry, and human medicine.
Full article
(This article belongs to the Special Issue Discovery and Synthesis of Antimicrobial Compounds Against Multidrug Resistance)
►▼
Show Figures
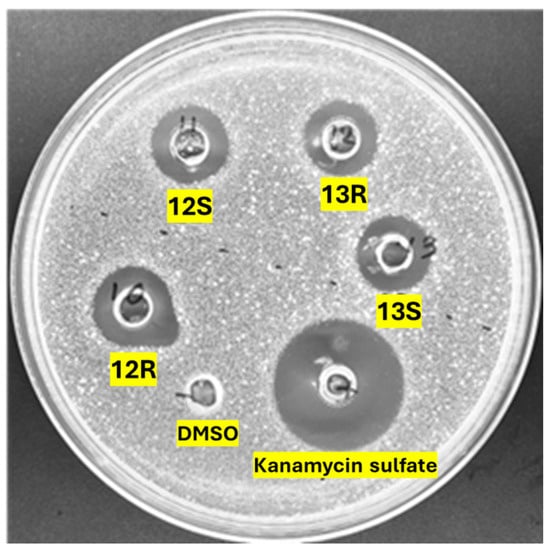
Figure 1
Open AccessArticle
Phenolic-Rich Wine Pomace Extracts as Antioxidant and Antipathogenic Agents Against Pseudomonas aeruginosa
by
Carolina María Viola, Mariana Elizabeth Danilovich, Romina Torres-Carro, Manuela M. Moreira, Francisca Rodrigues, Elena Cartagena, María Rosa Alberto, María Amparo Blázquez and Mario Eduardo Arena
Antibiotics 2025, 14(4), 384; https://doi.org/10.3390/antibiotics14040384 (registering DOI) - 5 Apr 2025
Abstract
►▼
Show Figures
Background/Objectives: Wine pomace is a rich source of bioactive phenolic compounds with potential health benefits. This study aimed to evaluate the antipathogenic and antioxidant properties of ethanol and ethyl acetate extracts from wine pomace of three grape varietals (Tannat, Bonarda, and Malbec) to
[...] Read more.
Background/Objectives: Wine pomace is a rich source of bioactive phenolic compounds with potential health benefits. This study aimed to evaluate the antipathogenic and antioxidant properties of ethanol and ethyl acetate extracts from wine pomace of three grape varietals (Tannat, Bonarda, and Malbec) to explore their potential as natural alternatives for mitigating bacterial virulence in Pseudomonas aeruginosa. Methods: Successive exhaustion extractions were performed using solvents of increasing polarity (ethyl acetate and ethanol). The phenolic content was quantified, and the antioxidant activity was evaluated using standard assays. The antipathogenic activity against P. aeruginosa was assessed by measuring biofilm formation, elastase and protease activity, pyocyanin production, and swarming motility. Quorum sensing (QS) inhibition was tested using a violacein production assay in Chromobacterium violaceum. Results: Ethanol was more effective at extracting phenolic compounds, with Tannat exhibiting the highest total phenolic content (162.5 µg GAE/mg). HPLC-DAD analysis identified 16 phenolic acids, 18 flavonoids, and 3 stilbenes across the extracts. The ethanol extracts showed strong antioxidant activity (phosphomolybdenum reducing capacity 67–128 μg AAE/mg, ABTS•+ scavenging 37–71 µg/mL, Fe3+ reducing power 31–68 µg/mL) and inhibited biofilm formation (up to 61%), elastase (up to 41%), and protease (up to 46%) activities in P. aeruginosa. The extracts also reduced pyocyanin production (up to 78%) and swarming motility (up to 68%), suggesting interference with QS. Moreover, the extracts inhibited violacein production in C. violaceum, confirming QS inhibition (up to 26%). Conclusions: Among the extracts, ethanol-extracted Tannat pomace showed the most substantial antipathogenic and antioxidant activities. The results add value to wine pomace by suggesting its use as natural extracts rich in phenolic compounds, capable of controlling the bacterial virulence of Pseudomonas aeruginosa without promoting the development of resistance.
Full article
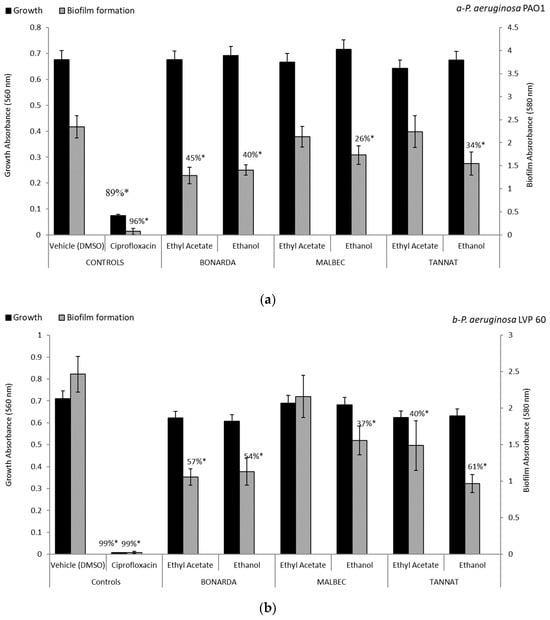
Figure 1
Open AccessArticle
Mechanism Insight of Cell Death Signaling by Thymol Derivatives on Trypanosmatidae Protozoan Parasites
by
Amani Omrani, Meriam Ben Youssef, Ines Sifaoui, Eduardo Hernández-Álvarez, Carlos J. Bethencourt-Estrella, Isabel L. Bazzocchi, Hichem Sebai, Jacob Lorenzo-Morales, Ignacio A. Jiménez and José E. Piñero
Antibiotics 2025, 14(4), 383; https://doi.org/10.3390/antibiotics14040383 (registering DOI) - 5 Apr 2025
Abstract
Leishmaniasis and Chagas disease are parasitic diseases considered to be among the most important neglected diseases, with implications for both developed and developing countries. Currently, there are no effective therapeutic treatments for these diseases due to challenges in drug administration, high toxicity, high
[...] Read more.
Leishmaniasis and Chagas disease are parasitic diseases considered to be among the most important neglected diseases, with implications for both developed and developing countries. Currently, there are no effective therapeutic treatments for these diseases due to challenges in drug administration, high toxicity, high costs, and drug resistance. In this study, a series of eleven thymol derivatives were designed, synthesized, and evaluated for their in vitro kinetoplastid activity against Leishmania amazonensis and Trypanosoma cruzi, as well as their cytotoxicity against a murine macrophage cell line. The most active compounds, thymol anysoate (9) and thymol picolinate (10), displayed the highest kinetoplastid activity with IC50 values of 22.87 and 25.16 µM against L. amazonensis and T. cruzi, respectively. Notably, both compounds demonstrated an excellent selectivity index against the mammal cell line. Structure–activity relationship studies revealed that the ester group plays a crucial role in activity. The most promising derivatives, 9 and 10, activate autophagy and apoptosis-like processes in the treated cells. Atomic force microscopy observations showed that derivative 9 induces the formation of cytoplasmic vacuoles, indicating an autophagic process, and drug-likeness analysis revealed that it meets all the pharmacokinetic criteria. Overall, these results highlight derivative 9 as a potential lead compound for the development of new drugs for the treatment of Trypanosomatidae infections and warrants further studies to elucidate the cell death cascade involved.
Full article
(This article belongs to the Collection Synthetic and Natural Products-Based Antimicrobial and Antiparasitic Agents)
►▼
Show Figures

Graphical abstract
Open AccessArticle
Characterization of Enterobacter cloacae and Citrobacter freundii Species Complex Isolates with Decreased Susceptibility to Cephalosporins from United States Hospitals and Activity of Aztreonam–Avibactam and Comparator Agents (2019–2023)
by
Helio S. Sader, Timothy B. Doyle, John H. Kimbrough, Rodrigo E. Mendes and Mariana Castanheira
Antibiotics 2025, 14(4), 382; https://doi.org/10.3390/antibiotics14040382 (registering DOI) - 5 Apr 2025
Abstract
►▼
Show Figures
Background: Citrobacter freundii (CFC) and Enterobacter cloacae (ECLC) species complexes represent important causes of hospital-associated infections, frequently are related to outbreaks, and have a great ability to develop antimicrobial resistance. We evaluated a large collection of CFC and ECLC isolates with decreased susceptibility
[...] Read more.
Background: Citrobacter freundii (CFC) and Enterobacter cloacae (ECLC) species complexes represent important causes of hospital-associated infections, frequently are related to outbreaks, and have a great ability to develop antimicrobial resistance. We evaluated a large collection of CFC and ECLC isolates with decreased susceptibility to broad-spectrum cephalosporins (Ceph-DS) from United States (US) hospitals. Methods: A total of 43,325 Enterobacterales (1/patient) were collected in 2019–2023 and susceptibility tested by broth microdilution; among those, 5106 (11.8%) were CFC (n = 1374) or ECLC (n = 3732). Ceph-DS CFC (n = 379) and ECLC isolates (n = 1065), defined as isolates with ceftazidime MICs ≥ 16 mg/L and/or cefepime MICs ≥ 2 mg/L, were screened for β-lactamase genes by whole genome sequencing. Results: The most common ESBLs were CTX-M type (n = 98; 47.6% of ESBL producers), SHV type (n = 94; 45.6%), and OXA type (n = 78; 37.9%); ≥2 ESBLs were identified in 65 isolates (31.6%), mainly OXA-1/30 plus a CTX-M. A carbapenemase was identified in 55 of 64 (85.9%) carbapenem-resistant (CB-R) isolates, including KPC type (40 isolates; 62.5% of CB-R) and NDM-1 (16; 23.4% of CB-R). Aztreonam–avibactam was active against 99.6% of Ceph-DS and 100.0% of ESBL producers and CB-R isolates, including NDM producers. Ceftazidime–avibactam and meropenem–vaborbactam were active against 100.0% of ESBL producers (excluding carbapenemase co-producers) and 70.3–71.9% of CB-R isolates. Cefiderocol was active against 82.8% of CB-R isolates but only 46.7% of MBL producers. Conclusions: Aztreonam–avibactam was highly active against cephalosporin-nonsusceptible ECLC and CFC, including MBL producers. The activities of ceftazidime–avibactam, meropenem–vaborbactam, and cefiderocol were compromised against CB-R isolates due to the high frequency of NDM producers.
Full article

Figure 1
Open AccessArticle
Design and Validation of a Simplified Method to Determine Minimum Bactericidal Concentration in Nontuberculous Mycobacteria
by
Sara Batista, Mariana Fernández-Pittol, Lorena San Nicolás, Diego Martínez, Sofía Narváez, Mateu Espasa, Elena Garcia Losilla, Marc Rubio, Montserrat Garrigo, Griselda Tudó and Julian González-Martin
Antibiotics 2025, 14(4), 381; https://doi.org/10.3390/antibiotics14040381 (registering DOI) - 4 Apr 2025
Abstract
Background/Objectives: Nontuberculous mycobacteria (NTM) infections are rising, particularly those by Mycobacterium avium complex (MAC) and Mycobacterium abscessus complex (MAB). Treating NTM infections is challenging due to their poor response to antibiotics. This study aimed to optimize the treatment of NTM infection by selecting
[...] Read more.
Background/Objectives: Nontuberculous mycobacteria (NTM) infections are rising, particularly those by Mycobacterium avium complex (MAC) and Mycobacterium abscessus complex (MAB). Treating NTM infections is challenging due to their poor response to antibiotics. This study aimed to optimize the treatment of NTM infection by selecting antibiotics with bactericidal activity for combination therapy. To do this, we used the minimum bactericidal concentration (MBC) determination approach to define bactericidal or bacteriostatic activity. We developed three main objectives: validate a new method to determine MBC based on a reincubation method, determine MBC values of 229 NTM clinical isolates using the reincubation method, and evaluate antibiotic stability in preincubated microtiter plates. Methods: First, we assessed the stability of the antibiotics included in SLOWMYCOI Sensititre™ microtiter plates. Five strains of MAC were studied comparing the minimum inhibitory concentrations (MICs) of those preincubated for seven days vs. non-incubated plates. Then, we evaluated the percentage of reproducibility of MBC values using two methods, reincubation and subculturing (standard or traditional method) in 30 MAC isolates. Finally, we validated the reincubation method and prospectively determined the MBC values of the 229 NTM clinical strains. Results: Antibiotic stability: The MIC was equivalent after 7 and 14 days for all the antibiotics, except rifampicin, for which the MIC increased by 2- to 3-fold after preincubation. Reincubation method: The percentage of reproducibility of the MBC values between the two methods was 95.2% (range 76.6% to 100%). Prospective validation: MBC/MIC ratios revealed differential bactericidal activity for most antibiotics according to the different species, being bactericidal in M. avium and Mycobacterium xenopi, and predominantly bacteriostatic in MAB. Conclusions: Preincubation of Sensititre™ microtiter plates did not alter the MIC values of the antibiotics included except for rifampicin, suggesting a loss of activity. MBC determination can be easily performed by the Reincubation method presented. MBC values provide useful additional information regarding MIC values since the MBC/MIC ratio reveals whether antibiotics have bactericidal or bacteriostatic activity according to the species, which is pivotal for selecting the most adequate antibiotic combination to ensure efficient treatment management.
Full article
(This article belongs to the Section Antibiotic Therapy in Infectious Diseases)
►▼
Show Figures
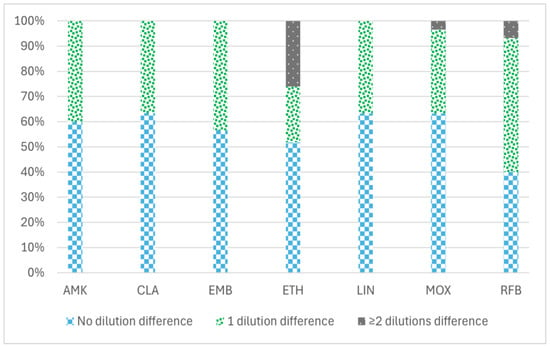
Figure 1
Open AccessArticle
One Health Approach: Antibiotic Resistance Among Enterococcal Isolates in Dairy Farms in Selangor
by
Sakshaleni Rajendiran, Yuvaneswary Veloo, Salina Abdul Rahman, Rohaida Ismail, Zunita Zakaria, Rozaihan Mansor, Maslina Mohd Ali, Hassuzana Khalil and Syahidiah Syed Abu Thahir
Antibiotics 2025, 14(4), 380; https://doi.org/10.3390/antibiotics14040380 (registering DOI) - 4 Apr 2025
Abstract
Background/Objectives: Antibiotic resistance is a growing public health concern. The One Health approach is essential in addressing antibiotic (AR) resistance. Therefore, this study aimed to determine AR among enterococcal isolates in dairy farms across various domains based on the emerging dairy industry. Methods:
[...] Read more.
Background/Objectives: Antibiotic resistance is a growing public health concern. The One Health approach is essential in addressing antibiotic (AR) resistance. Therefore, this study aimed to determine AR among enterococcal isolates in dairy farms across various domains based on the emerging dairy industry. Methods: A total of 208 enterococcal isolates from the workers = 70, milk = 76, and environment = 62 of eight dairy farms in Selangor, Malaysia, were used in this study. The bacterial identification and antibiotic susceptibility testing (AST) were conducted utilising the Vitek-2 system. Results: Approximately 28% of the isolates exhibited susceptibility to all tested antibiotics. A relatively higher proportion of isolates demonstrated resistance to tetracycline, which was followed by erythromycin. The multidrug resistance (MDR) and multiple antibiotic resistance (MAR) index were low in this study. Conclusions: The studied dairy farms exhibited lower AR, MDR, and MAR index values. Nevertheless, ongoing surveillance is essential due to the recent expansion of the dairy farming industry.
Full article
(This article belongs to the Special Issue Antibiotic Resistance: A One-Health Approach, 2nd Edition)
►▼
Show Figures

Figure 1
Open AccessReview
Harnessing the Power of Antimicrobial Peptides: From Mechanisms to Delivery Optimization for Topical Infections
by
Songhita Mukhopadhyay, Souha H. Youssef, Yunmei Song, Usha Y. Nayak and Sanjay Garg
Antibiotics 2025, 14(4), 379; https://doi.org/10.3390/antibiotics14040379 (registering DOI) - 4 Apr 2025
Abstract
Antimicrobial peptides (AMPs) have emerged as promising agents for treating topical infections due to their enhanced biocompatibility and resistance to systemic degradation. AMPs possess host immunomodulatory effects and disintegrate bacterial cell membranes, a mechanism less prone to microbial resistance compared to conventional antibiotics,
[...] Read more.
Antimicrobial peptides (AMPs) have emerged as promising agents for treating topical infections due to their enhanced biocompatibility and resistance to systemic degradation. AMPs possess host immunomodulatory effects and disintegrate bacterial cell membranes, a mechanism less prone to microbial resistance compared to conventional antibiotics, making AMPs potential candidates for antimicrobial delivery. The review discusses the challenges posed by antimicrobial resistance (AMR) and explores the mechanisms by which bacteria develop resistance to AMPs. The authors provide a detailed analysis of the mechanisms of action of AMPs, their limitations, and strategies to improve their efficacy. Conventional AMP delivery systems, including polymeric, synthetic, and lipid-based nanoparticles and cubosomes, face challenges of microbial resistance mechanisms via efflux pump systems, bacterial cell membrane modifications, and protease enzyme release. This review explores strategies to optimize these delivery systems. Furthermore, market statistics and the growing interest in peptide antibiotics have been explored in this review. The authors provide future research directions, such as exploring gene-targeting approaches to combat emerging bacterial resistance against AMPs, and emphasize considering the conformational stability of peptides, the skin microbiome’s nature at the infection site, and proteolytic stability for developing efficient AMP delivery systems for topical infections.
Full article
(This article belongs to the Collection Synthetic and Natural Products-Based Antimicrobial and Antiparasitic Agents)
►▼
Show Figures

Graphical abstract
Open AccessArticle
A Prospective Analysis of the Burden of Multi-Drug-Resistant Pathogens in Acute Appendicitis and Their Implication for Clinical Management
by
Faruk Koca, Sara Fatima Faqar-Uz-Zaman, Claudia Reinheimer, Michael Hogardt, Volkhard A. J. Kempf, Paul Ziegler, Andreas A. Schnitzbauer, Armin Wiegering, Wolf Otto Bechstein and Patrizia Malkomes
Antibiotics 2025, 14(4), 378; https://doi.org/10.3390/antibiotics14040378 - 4 Apr 2025
Abstract
Background/Objectives: Appendicitis caused by multi-drug-resistant pathogens is associated with significant postoperative morbidity. However, prospective data on the microbial spectrum and its clinical impact remain limited. Methods: Adults with acute appendicitis undergoing surgery between April 2022 and July 2023 were prospectively enrolled
[...] Read more.
Background/Objectives: Appendicitis caused by multi-drug-resistant pathogens is associated with significant postoperative morbidity. However, prospective data on the microbial spectrum and its clinical impact remain limited. Methods: Adults with acute appendicitis undergoing surgery between April 2022 and July 2023 were prospectively enrolled at a single university-affiliated institution. Bacterial cultures from appendiceal and rectal swabs were analyzed, and clinical outcomes were assessed. A telephone follow-up was conducted 30 days postoperatively. Results: A total of 105 patients were included. Multi-drug-resistant pathogens were identified in the appendiceal swabs of twenty-nine patients (27.6%), while six patients (5.7%) harbored multi-drug-resistant organisms (MDROs; according to the criteria of the CDC). Rectal swabs revealed MDROs in 11.4% of cases but showed a limited correlation with appendiceal samples, indicating that rectal colonization does not reliably predict the presence of MDROs in appendicitis. Patients with multi-drug-resistant infections had significantly higher postoperative complication rates (31% vs. 10.5%, p = 0.017), including more Clavien–Dindo grade 3 complications (17.2% vs. 2.6%, p = 0.007) and abdominal abscesses (10.3% vs. 1.3%, p = 0.03). These patients required more frequent postoperative antibiotic treatment (65.5% vs. 40.8%, p = 0.03) and therapy adjustments (37.9% vs. 15.8%, p = 0.02). Hospital stays were also prolonged in the multi-drug-resistant group (a median of 4 days and IQR of 5 days vs. a median of 3 days and IQR of 3 days; p = 0.03). Conclusions: Colonization with multi-drug-resistant pathogens in appendicitis is associated with worse clinical outcomes. The intraoperative microbiological analysis of appendiceal swabs in complicated cases may enable targeted antibiotic therapy, potentially shortening hospital stays, optimizing patient management and reducing healthcare costs.
Full article
(This article belongs to the Section Antibiotic Therapy in Infectious Diseases)
Open AccessArticle
Antimicrobial Resistance Patterns of ESBL-Producing Escherichia coli in Dogs from Thailand: Evaluation of Algal Extracts as Novel Antimicrobial Agents
by
Khomson Satchasataporn, Duangdaow Khunbutsri, Peechanika Chopjitt, Samak Sutjarit, Wanida Pan-utai and Nattakan Meekhanon
Antibiotics 2025, 14(4), 377; https://doi.org/10.3390/antibiotics14040377 - 3 Apr 2025
Abstract
Background/Objectives: Multidrug-resistant (MDR) bacteria, including extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli, in companion animals pose a growing public health concern due to the close interactions between pets and humans. This study aimed to investigate antimicrobial resistance patterns and the prevalence of ESBL-producing E.
[...] Read more.
Background/Objectives: Multidrug-resistant (MDR) bacteria, including extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli, in companion animals pose a growing public health concern due to the close interactions between pets and humans. This study aimed to investigate antimicrobial resistance patterns and the prevalence of ESBL-producing E. coli isolated from healthy dogs in Thailand, as well as the potential of algal extracts obtained through ethanol extraction and enzymatic hydrolysis as alternative antimicrobial agents against these drug-resistant organisms. Methods: Antimicrobial susceptibility testing was performed on 43 E. coli isolates from healthy dogs. ESBL production was confirmed using standard phenotypic methods, and resistance genes were detected by PCR. The algal extracts were tested for antibacterial activity against MDR isolates. Results: Among the 43 E. coli isolates, 67.44% were classified as MDR, with high resistance rates observed for ampicillin (79.07%), tetracycline (65.12%), and ciprofloxacin (62.79%), highlighting significant antimicrobial resistance concerns. Of the MDR isolates, 31.03% (9/29) were confirmed as ESBL producers. Gene analysis revealed blaTEM as the most prevalent gene (53.49%), followed by blaCTX-M (9.30%), while blaSHV was detected in a single isolate resistant only to ampicillin and was absent in all MDR strains. Ethanol extracts of Haematococcus pluvialis and Caulerpa lentillifera demonstrated inhibitory effects against MDR E. coli. Conclusions: MDR and ESBL-producing E. coli are prevalent in healthy dogs, posing a potential public health risk. Algal extracts from H. pluvialis and C. lentillifera show promise as alternative antimicrobials. Further research is necessary to optimize their efficacy and investigate their in vivo applications, including clinical and environmental settings.
Full article
(This article belongs to the Special Issue Antimicrobial Resistance and Infections in Animals)
►▼
Show Figures

Figure 1
Open AccessArticle
Knowledge, Attitudes, and Practices of Iraqi Parents Regarding Antibiotic Use in Children and the Implications
by
Omeed Darweesh, Amanj Kurdi, Marwan Merkhan, Hemn Ahmed, Salih Ibrahem, Radhwan N. Al-Zidan, Johanna C. Meyer and Brian Godman
Antibiotics 2025, 14(4), 376; https://doi.org/10.3390/antibiotics14040376 (registering DOI) - 3 Apr 2025
Abstract
Background: Antibiotic misuse is a major global health issue, particularly in low- and middle-income countries (LMICs), where inappropriate use contributes to antimicrobial resistance (AMR). Inappropriate antibiotic use is exacerbated in LMICs by pressure from parents on physicians and pharmacists to prescribe and dispense
[...] Read more.
Background: Antibiotic misuse is a major global health issue, particularly in low- and middle-income countries (LMICs), where inappropriate use contributes to antimicrobial resistance (AMR). Inappropriate antibiotic use is exacerbated in LMICs by pressure from parents on physicians and pharmacists to prescribe and dispense antibiotics for their children, often for viral infections. There is currently limited knowledge of key issues in Iraq to improve future antibiotic use. Consequently, we explored knowledge, attitudes, and practices (KAPs) of Iraqi parents regarding antibiotic use in their children to provide future direction. Methods: A cross-sectional survey was conducted between November 2023 and September 2024 among 1878 parents in four districts of Iraq. A structured questionnaire assessed parents’ KAPs towards antibiotic-related uses and practices. Data were analyzed using descriptive statistics and Chi-square tests to examine the associations between demographic variables and KAP indicators. Results: Among the participants, 83% were aware that antibiotics are ineffective for viral infections, and 75% recognized potential side effects from antibiotics. Despite this knowledge, 63% of parents admitted to administering antibiotics to their children without a prescription, with 42% discontinuing treatment once symptoms improved. Factors including cost, dosage, and taste influenced antibiotic selection. Parents with higher education and income levels were more likely to engage in self-medication. Pharmacists were the primary source of antibiotic information for 52% of respondents. Conclusions: Despite adequate knowledge, inappropriate practices such as self-medication and discontinuing treatment early were prevalent. Targeted educational campaigns, particularly among parents with higher education levels and incomes, are necessary to mitigate AMR in Iraq.
Full article
(This article belongs to the Special Issue Knowledge, Attitudes and Practices of Antimicrobial Resistance and Stewardship in Primary Care Setting: From Understanding to Informing Interventions)
Open AccessArticle
Antibiotic Resistance in Lactic Acid Bacteria from Dairy Products in Northern Italy
by
Irene Floris, Roberta Battistini, Clara Tramuta, Aitor Garcia-Vozmediano, Noemi Musolino, Giulia Scardino, Chiara Masotti, Beatrice Brusa, Riccardo Orusa, Laura Serracca, Elisabetta Razzuoli, Francesca Martucci and Daniela Manila Bianchi
Antibiotics 2025, 14(4), 375; https://doi.org/10.3390/antibiotics14040375 (registering DOI) - 3 Apr 2025
Abstract
Background: The spread of antibiotic resistance genes (ARGs) from the food chain is a significant public health concern. Dairy products from raw milk containing lactic acid bacteria (LAB) resistant to antimicrobials may serve as vectors for the transfer of resistance to commensal
[...] Read more.
Background: The spread of antibiotic resistance genes (ARGs) from the food chain is a significant public health concern. Dairy products from raw milk containing lactic acid bacteria (LAB) resistant to antimicrobials may serve as vectors for the transfer of resistance to commensal or potentially pathogenic bacteria in the human gut. Detecting ARGs in dairy products and milk is, therefore, crucial and could aid in the development of strategies to mitigate resistance dissemination through the food chain. Objectives: This study aimed to determine the presence of ARGs and assess the antibiotic susceptibility of LAB strains isolated from dairy products made from raw milk. Methods: Fifty-four LAB strains were isolated from 41 dairy samples and were tested for antimicrobial susceptibility using broth microdilution to determine Minimal Inhibitory Concentration (MIC). Moreover, the presence of resistance genes related to tetracyclines, beta-lactams, quinolones, and erythromycin was examined using six multiplex PCR assays. Results: Lactobacillus spp. and Leuconostoc spp. strains exhibited a high level of resistance to vancomycin (93–100%). Low-level resistance (4.2–20%) was observed in Lactococcus spp. and Lactobacillus spp. strains against tetracycline. Additionally, Lactococcus spp. strains showed resistance to trimethoprim/sulfamethoxazole, erythromycin, and clindamycin. Twenty-two out of 54 LAB strains (40.7%) carried at least one antibiotic resistance gene, and five of these were multidrug-resistant. Genes associated with acquired resistance to tetracycline were commonly detected, with tetK being the most frequent determinant. Conclusions: This study demonstrated that LABs in dairy products can act as reservoirs for ARGs, potentially contributing to the horizontal transfer of resistance within microbial communities in food and consumers. These findings highlight the need for the ongoing surveillance of antibiotic resistance in LAB and the implementation of control measures to minimize the dissemination of resistance through dairy products.
Full article
(This article belongs to the Special Issue Microbial Resistance Surveillance and Management in Food Systems)
►▼
Show Figures

Figure 1
Open AccessArticle
Frog Skin Peptides Hylin-a1, AR-23, and RV-23: Promising Tools Against Carbapenem-Resistant Escherichia coli and Klebsiella pneumoniae Infections
by
Annalisa Chianese, Annalisa Ambrosino, Rosa Giugliano, Francesca Palma, Preetu Parimal, Marina Acunzo, Alessandra Monti, Nunzianna Doti, Carla Zannella, Massimiliano Galdiero and Anna De Filippis
Antibiotics 2025, 14(4), 374; https://doi.org/10.3390/antibiotics14040374 - 3 Apr 2025
Abstract
Background/Objectives. One of the pressing challenges in global public health is the rise in infections caused by carbapenem-resistant Enterobacteriaceae. Growing bacterial drug resistance, coupled with the slow development of new antibiotics, highlights the critical need to explore and develop new broad-spectrum antimicrobial agents
[...] Read more.
Background/Objectives. One of the pressing challenges in global public health is the rise in infections caused by carbapenem-resistant Enterobacteriaceae. Growing bacterial drug resistance, coupled with the slow development of new antibiotics, highlights the critical need to explore and develop new broad-spectrum antimicrobial agents able to inhibit bacterial growth efficiently. In recent years, antimicrobial peptides (AMPs) have gained significant attention as a promising alternative to conventional drugs, owing to their antimicrobial potency, low toxicity, and reduced propensity for fostering resistance. Our research aims to investigate the antibacterial ability of three amphibian AMPs, namely Hylin-a1, AR-23, and RV-23, against both antibiotic-sensitive and carbapenem-resistant strains of Escherichia coli and Klebsiella pneumoniae. Methods. A 3-(4,5 dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay (MTT) was performed to identify non-cytotoxic concentrations of peptides. A microdilution assay evaluated the antibacterial effect, determining the peptides’ minimum inhibitory concentration (MIC). In addition, the checkerboard test analyzed the compounds’ synergistic effect with meropenem. Results. We demonstrated that peptides with low toxicity profile and resistance to proteolytic activity exhibited strong antibacterial activity, with MIC ranging from 6.25 to 25 μM. The antibiofilm mechanism of action of peptides was also investigated, suggesting that they had a crucial role during the biofilm formation step by inhibiting it. Finally, we highlighted the synergistic effects of peptides with meropenem. Conclusions. Our study identifies Hylin-a1, AR-23, and RV-23 as promising candidates against Gram-negative bacterial infections with a favorable therapeutic profile. This effect could be related to their great flexibility, as evidenced by circular dichroism data, confirming that the peptides could assume an α-helical conformation interacting with bacterial membranes.
Full article
(This article belongs to the Special Issue Present and Future of Antibiotic Treatment for Carbapenem-Resistant Enterobacteriaceae)
►▼
Show Figures

Figure 1
Open AccessArticle
Piloting an Information and Communication Technology Tool to Help Addressing the Challenge of Antimicrobial Resistance in Low-Income Countries
by
Florence Mutua, Joshua Orungo Onono, Sofia Boqvist, Patricia Koech, Abdullahi M. Abdi, Hildah Karimi and Susanna Sternberg-Lewerin
Antibiotics 2025, 14(4), 373; https://doi.org/10.3390/antibiotics14040373 - 3 Apr 2025
Abstract
Background/Objectives: Antimicrobial use (AMU) in livestock drives antimicrobial resistance (AMR). AMR has a significant impact on public health. While several interventions have been used to address this challenge, few have utilized Information and Communication Technology (ICT) approaches. The objective of this study
[...] Read more.
Background/Objectives: Antimicrobial use (AMU) in livestock drives antimicrobial resistance (AMR). AMR has a significant impact on public health. While several interventions have been used to address this challenge, few have utilized Information and Communication Technology (ICT) approaches. The objective of this study was to pilot and assess an ICT system to monitor the use of veterinary drugs and disseminate information to farmers in peri-urban smallholder poultry systems in Kenya. Methods: The system was developed in collaboration with the stakeholders. It captures drug sales in veterinary pharmacies and disease incidence and treatments reported by farmers. The system was piloted from May 2023 to December 2023. Monthly follow-ups were conducted to monitor progress and address problems. Assessment was performed through focus group discussions with the users (two with farmers and two with veterinary pharmacy staff) and descriptive statistics of the data collected by the system. Results: A total of 15,725 records were obtained from veterinary pharmacies, including antibiotics (57%), dewormers (22%), and vitamins (11%). Requests for a specific product were recorded in 38% of the sales, while 63% were accompanied by some evidence (empty drug containers, old packages, old prescriptions, pictures of sick birds, and actual sick birds). A total of 91 records were obtained from the farmers. The health problems reported were mostly respiratory (40%) and digestive (30%) disorders. The percentage of customers who requested advice on animal health when visiting veterinary pharmacies ranged from 5 to 20%. Conclusions: AMU can be improved in the study area. The piloted system may help policymakers monitor the sales and usage of antibiotics, improve animal health management, and promote responsible AMU.
Full article
(This article belongs to the Special Issue Research Advances in Antimicrobial Stewardship, Residues and Resistance in Veterinary and Environmental Science)
►▼
Show Figures
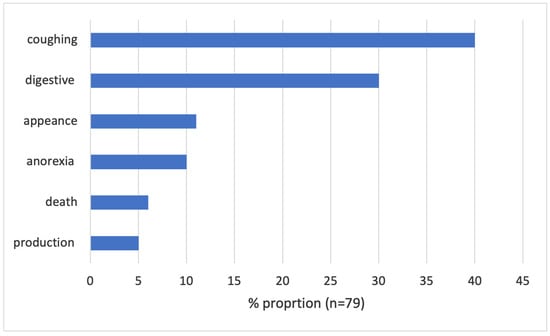
Figure 1
Open AccessArticle
Unexpected Positive Cultures During Aseptic Hip and Knee Revision Arthroplasty: Substantial Discrepancies in Laboratory Analyses
by
Marius Ludwig, Michael Fuchs, Olivia Trappe, Moritz Oltmanns, Heiko Reichel and Tobias Freitag
Antibiotics 2025, 14(4), 372; https://doi.org/10.3390/antibiotics14040372 - 3 Apr 2025
Abstract
Background: Microbial analysis of tissue samples represents an important diagnostic tool in the course of revision total joint arthroplasty. Currently, unexpected positive intraoperative cultures are commonly observed during presumed aseptic revision surgery and evoke a degree of uncertainty among physicians. To date, it
[...] Read more.
Background: Microbial analysis of tissue samples represents an important diagnostic tool in the course of revision total joint arthroplasty. Currently, unexpected positive intraoperative cultures are commonly observed during presumed aseptic revision surgery and evoke a degree of uncertainty among physicians. To date, it is unclear if there are deviations in pathogen detection between certified laboratories. Methods: Tissue samples of sixty consecutive patients undergoing presumably aseptic total hip and knee revision surgery were sent to two different internationally certified accredited laboratories and tested for any microbial growth as well as pathogen differentiation. Results: Each laboratory analyzed 300 samples. Laboratory 1 observed an unexpected positive culture rate of 16.7%; laboratory 2 indicated that 18.3% of all processed specimens showed pathogen growth. In comparison, a consistent microbial evaluation was only present in one patient. The kappa correlation coefficient showed a poor correlation between the two laboratories in all evaluated categories. Coagulase-negative staphylococci represented the most common pathogens of laboratory 1, while laboratory 2 predominantly observed cutibacterium acnes species. Within a mean follow-up period of 17.6 ± 18.6 months (range: 0–63 months), there was no revision due to periprosthetic joint infection. Conclusions: Unexpected positive culture results during presumed aseptic revision surgery remain a significant clinical challenge. This study is the first of its kind to evaluate the convergence of laboratory findings in the context of aseptic revision surgery. Our results suggest that even established and certified laboratories show substantial discrepancies. Thus, a careful interpretation of unexpected bacterial cultures after revision surgery is mandatory. Given the uncertainty inherent in laboratory findings, a precise clinical and histopathological evaluation of this patient cohort should be ensured.
Full article
(This article belongs to the Special Issue Prevention, Diagnostic and Antibiotic Treatment of Periprosthetic Joint and Fracture Related Infection, 2nd Edition)
Open AccessReview
The Impact of Antibiotic Therapy on Intestinal Microbiota: Dysbiosis, Antibiotic Resistance, and Restoration Strategies
by
Gaia Cusumano, Giancarlo Angeles Flores, Roberto Venanzoni and Paola Angelini
Antibiotics 2025, 14(4), 371; https://doi.org/10.3390/antibiotics14040371 - 3 Apr 2025
Abstract
The human gut microbiota—an intricate and dynamic ecosystem—plays a pivotal role in metabolic regulation, immune modulation, and the maintenance of intestinal barrier integrity. Although antibiotic therapy is indispensable for managing bacterial infections, it profoundly disrupts gut microbial communities. Such dysbiosis is typified by
[...] Read more.
The human gut microbiota—an intricate and dynamic ecosystem—plays a pivotal role in metabolic regulation, immune modulation, and the maintenance of intestinal barrier integrity. Although antibiotic therapy is indispensable for managing bacterial infections, it profoundly disrupts gut microbial communities. Such dysbiosis is typified by diminished diversity and shifts in community structure, especially among beneficial bacterial genera (e.g., Bifidobacterium and Eubacterium), and fosters antibiotic-resistant strains and the horizontal transfer of resistance genes. These alterations compromise colonization resistance, increase intestinal permeability, and amplify susceptibility to opportunistic pathogens like Clostridioides difficile. Beyond gastrointestinal disorders, emerging evidence associates dysbiosis with systemic conditions, including chronic inflammation, metabolic syndrome, and neurodegenerative diseases, underscoring the relevance of the microbiota–gut–brain axis. The recovery of pre-existing gut communities post-antibiotic therapy is highly variable, influenced by drug spectrum, dosage, and treatment duration. Innovative interventions—such as fecal microbiota transplantation (FMT), probiotics, synbiotics, and precision microbiome therapeutics—have shown promise in counteracting dysbiosis and mitigating its adverse effects. These therapies align closely with antibiotic stewardship programs aimed at minimizing unnecessary antibiotic use to preserve microbial diversity and curtail the spread of multidrug-resistant organisms. This review emphasizes the pressing need for microbiota-centered strategies to optimize antibiotic administration, promote long-term health resilience, and alleviate the disease burden associated with antibiotic-induced dysbiosis.
Full article
(This article belongs to the Special Issue Antibiotics as Major Disruptors of Gut Microbiota)
►▼
Show Figures

Figure 1
Open AccessReview
Nebulized Antibiotics for Preventing and Treating Gram-Negative Respiratory Infections in Critically Ill Patients: An Overview of Reviews
by
Marios Karvouniaris, Despoina Koulenti, Konstantinos I. Bougioukas, Eirini Pagkalidou, Elizabeth Paramythiotou and Anna-Bettina Haidich
Antibiotics 2025, 14(4), 370; https://doi.org/10.3390/antibiotics14040370 - 2 Apr 2025
Abstract
►▼
Show Figures
Background. Ventilator-associated tracheobronchitis (VAT) and pneumonia (VAP) are the most frequent nosocomial infections in the critical care setting and are associated with increased morbidity. At the same time, VAP is also associated with attributable mortality, especially when caused by difficult-to-treat (DTR) Gram-negative bacteria
[...] Read more.
Background. Ventilator-associated tracheobronchitis (VAT) and pneumonia (VAP) are the most frequent nosocomial infections in the critical care setting and are associated with increased morbidity. At the same time, VAP is also associated with attributable mortality, especially when caused by difficult-to-treat (DTR) Gram-negative bacteria (GNB) that have limited treatment options. Studies have assessed the impact of nebulized aminoglycosides or colistin to improve VAT and VAP outcomes or as an adjunct to intravenous antimicrobial treatment or as a preventive approach. Objective. This overview aimed to assess systematic reviews that examine the efficacy and safety of antimicrobial nebulization for preventing and treating ventilator-associated infections in the critically ill. Methods. Systematic reviews, meta-analyses, and original randomized controlled trials and prospective observational studies were included. Searches were conducted in MEDLINE (via PubMed), the Cochrane, Epistemonikos, and PROSPERO. The methodological quality assessment was performed using standardized tools. Results. Regarding VAP treatment, the included systematic reviews presented critically low quality. The clinical response effect size to amikacin and colistin nebulization were RR 1.23 (95% CI 1.13–1.34), I2 = 47% and OR 1.39 (0.87–2.20), I2 = 56%. The main safety concern was bronchospasm with RR 2.55 (1.40–4.66), I2 = 0% and OR 5.19 (1.05–25.52), I2 = 0%. The certainty of evidence was usually very low. For VAT treatment, limited evidence showed a better clinical response and less emergence of resistant bacteria. Regarding VAP prevention, data are limited to two trials; however, only the larger one presented a low risk of bias and resulted in a reduced VAP rate. Conclusions. Delivery via nebulization might be considered in addition to IV antimicrobial treatment of GNB ventilator-associated infections. The available evidence is weak, and more studies focused on infections due to DTR-GNBs should be prioritized.
Full article

Figure 1
Open AccessCorrection
Correction: Domán et al. Comparative Genome Analysis of Canine Frederiksenia canicola Isolates. Antibiotics 2024, 13, 1235
by
Marianna Domán, Krisztina Pintér, Boglárka Dóra Pollák, Ágnes Pintér, Enikő Wehmann, Miklós Tenk and Tibor Magyar
Antibiotics 2025, 14(4), 369; https://doi.org/10.3390/antibiotics14040369 - 2 Apr 2025
Abstract
In the published publication [...]
Full article
(This article belongs to the Section Genetic and Biochemical Studies of Antibiotic Activity and Resistance)
Open AccessArticle
Indwelling Catheters Should Be Restricted in Primary and Revision Arthroplasty: A Retrospective Analysis After Changes to Hospital Standard Perioperative Treatment Protocol
by
Matthias Schnetz, Tim Jakobi, Larissa Ewald, Alexander Klug, Matthias Münzberg and Yves Gramlich
Antibiotics 2025, 14(4), 368; https://doi.org/10.3390/antibiotics14040368 - 2 Apr 2025
Abstract
Background: Indwelling catheters are used in the perioperative management of patients treated with total joint arthroplasty (TJA) to facilitate fluid control, ease postoperative miction until patients are able to ambulate, and prevent postoperative urinary retention (POUR). However, in TJA, they may be associated
[...] Read more.
Background: Indwelling catheters are used in the perioperative management of patients treated with total joint arthroplasty (TJA) to facilitate fluid control, ease postoperative miction until patients are able to ambulate, and prevent postoperative urinary retention (POUR). However, in TJA, they may be associated with a higher risk of urinary tract infections (UTIs). The aim of the study was to analyze the rates of urinary tract infections and POUR. Methods: Between 2021 and 2022, this study retrospectively identified patients before and after a change in the hospital standard perioperative treatment protocol towards a more restrictive use of indwelling catheters for TJA. In 2021, the use of indwelling catheters involved standard care, but the use was restricted in 2022. Results: A total of 1521 patients were included: 636 patients (41.8%) underwent primary arthroplasty, 646 (42.5%) underwent revision arthroplasty, and 239 (15.7%) underwent hip arthroplasty for femoral neck fractures. Standard use of indwelling catheters significantly decreased from 62.0% to 38.0% (p < 0.001), and the rate of UTI was significantly lower after the protocol change (4.7% vs. 1.2%; p < 0.001). Perioperative urine catheterization was a significant risk factor for UTI (OR = 4.22; p < 0.001), and UTI was a significant risk factor for PJI (OR = 9.99; p < 0.001). POUR increased slightly from 0.9% to 1.8%, but the difference was not significant. POUR was mostly diagnosed following the exchange of the acetabular component in revision arthroplasty (n = 11; 52.4%). Conclusions: Indwelling catheter use was associated with high rates of UTIs. Restricting perioperative use of indwelling catheters was effective in preventing UTIs while causing only a moderate increase in easily treatable postoperative urinary retention. Therefore, the use of indwelling catheters should be avoided in arthroplasty whenever possible.
Full article
(This article belongs to the Special Issue Prevention, Diagnostic and Antibiotic Treatment of Periprosthetic Joint and Fracture Related Infection, 2nd Edition)
►▼
Show Figures

Figure 1

Journal Menu
► ▼ Journal Menu-
- Antibiotics Home
- Aims & Scope
- Editorial Board
- Reviewer Board
- Topical Advisory Panel
- Instructions for Authors
- Special Issues
- Topics
- Sections & Collections
- Article Processing Charge
- Indexing & Archiving
- Editor’s Choice Articles
- Most Cited & Viewed
- Journal Statistics
- Journal History
- Journal Awards
- Society Collaborations
- Conferences
- Editorial Office
Journal Browser
► ▼ Journal BrowserHighly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Antibiotics, Biomedicines, JCM, Pharmaceuticals, Pharmaceutics
Challenges and Future Prospects of Antibacterial Therapy
Topic Editors: Kwang-sun Kim, Zehra EdisDeadline: 30 June 2025
Topic in
Antibiotics, Antioxidants, JoF, Microbiology Research, Microorganisms
Redox in Microorganisms, 2nd Edition
Topic Editors: Michal Letek, Volker BehrendsDeadline: 31 July 2025
Topic in
Agriculture, Animals, Veterinary Sciences, Antibiotics, Zoonotic Diseases
Animal Diseases in Agricultural Production Systems: Their Veterinary, Zoonotic, and One Health Importance, 2nd Edition
Topic Editors: Ewa Tomaszewska, Beata Łebkowska-Wieruszewska, Tomasz Szponder, Joanna Wessely-SzponderDeadline: 30 September 2025
Topic in
Antibiotics, JPM, Pharmaceuticals, Pharmaceutics, Medicines
Pharmacokinetic and Pharmacodynamic Modelling in Drug Discovery and Development
Topic Editors: Inaki F. Troconiz, Victor Mangas Sanjuán, Maria Garcia-Cremades MiraDeadline: 31 October 2025

Conferences
26–29 August 2025
The 5th International Symposium on Frontiers in Molecular Science
Molecular Regulatory Mechanisms of Biological Function and Drug Discovery based on Protein Structure/Function Analysis
Molecular Regulatory Mechanisms of Biological Function and Drug Discovery based on Protein Structure/Function Analysis

21–23 May 2025
The 4th International Electronic Conference on Antibiotics: Challenges and Strategies for the Antibiotic Resistance Crisis

Special Issues
Special Issue in
Antibiotics
Comprehensively Addressing Antimicrobial Resistance, Improving Food Safety and Achieving the One Health Goals: Global Challenges
Guest Editors: Vladimir Kurćubić, Pavle Mašković, Milan Mitić, Nikola StanišićDeadline: 15 April 2025
Special Issue in
Antibiotics
Discovery and Synthesis of Antimicrobial Compounds Against Multidrug Resistance
Guest Editor: Anita CohenDeadline: 15 April 2025
Special Issue in
Antibiotics
Nanotechnology-Based Antimicrobials and Drug Delivery Systems
Guest Editors: Mihai Valentin Predoi, Simona Iconaru, Carmen Steluta CiobanuDeadline: 15 April 2025
Special Issue in
Antibiotics
Antimicrobial Stewardship in the Digital Age: The Role of Artificial Intelligence and Chatbots in Future Strategies
Guest Editor: Alessandro PerrellaDeadline: 15 April 2025
Topical Collections
Topical Collection in
Antibiotics
Antibiotics in Ophthalmology Practice
Collection Editor: Sanjay Marasini
Topical Collection in
Antibiotics
Staphylococcus— Molecular Pathogenesis, Virulence Regulation and Antibiotics Resistance
Collection Editor: Ewa Szczuka
Topical Collection in
Antibiotics
Editorial Board Members' Collection Series: Structural Aspects of AMPs and Antimicrobials
Collection Editors: J. Michael Conlon, Marc Maresca, Bong-Jin Lee, Aurélie Tasiemski
Topical Collection in
Antibiotics
Synthetic and Natural Products-Based Antimicrobial and Antiparasitic Agents
Collection Editor: Antonio Eduardo Miller Crotti








