Journal Description
Dermatopathology
Dermatopathology
is an international, peer-reviewed, open access journal on dermatopathology. The journal is owned by the European Society of Dermatopathology (ESDP) and is published quarterly online by MDPI (since Volume 7 Issue 1 - 2020).
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High visibility: indexed within ESCI (Web of Science), PubMed, PMC, Embase, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 34.6 days after submission; acceptance to publication is undertaken in 3.6 days (median values for papers published in this journal in the second half of 2024).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
1.6 (2023);
5-Year Impact Factor:
1.3 (2023)
Latest Articles
Dermatomyositis-like Eruptions, Hydroxyurea-Associated Squamous Dysplasia, and Nonmelanoma Skin Cancer: A Case Report and Systematic Review
Dermatopathology 2025, 12(2), 11; https://doi.org/10.3390/dermatopathology12020011 - 30 Mar 2025
Abstract
Hydroxyurea (HU), a cornerstone treatment for myeloproliferative disorders, is associated with a wide range of cutaneous side effects, from xerosis and hyperpigmentation to more severe conditions like dermatomyositis-like eruptions (DM-LE) and nonmelanoma skin cancers (NMSC), particularly squamous cell carcinoma (SCC). In this review,
[...] Read more.
Hydroxyurea (HU), a cornerstone treatment for myeloproliferative disorders, is associated with a wide range of cutaneous side effects, from xerosis and hyperpigmentation to more severe conditions like dermatomyositis-like eruptions (DM-LE) and nonmelanoma skin cancers (NMSC), particularly squamous cell carcinoma (SCC). In this review, we present a unique case of HU-induced DM-LE with histological evidence of keratinocyte dysplasia and p53 overexpression, followed by a systematic analysis of similar cases. Our findings reveal that the clinical presentation of DM-LE, while typically considered benign, shares clinical and histological features with hydroxyurea-associated squamous dysplasia (HUSD), a precancerous condition that may progress to SCC in chronically exposed patients. Key insights include the characteristic histopathological findings of DM-LE, the role of chronic HU therapy and UV-induced damage in promoting p53 overexpression, and the overlap between DM-LE and HUSD. Regular dermatologic monitoring, patient education on photoprotection, and the careful assessment of skin lesions in long-term HU users are essential for the early detection and prevention of malignancies. This review underscores the importance of distinguishing between DM-LE, HUSD, and SCC to optimize management and minimize risks associated with HU therapy.
Full article
(This article belongs to the Section Clinico-Pathological Correlation in Dermatopathology)
►
Show Figures
Open AccessCase Report
Uncommon Collision Tumors: Dermoscopic and Histopathological Features of Basal Cell Carcinoma Overlying Dermatofibroma
by
Amal Makansi, Charlotta Enerbäck, Maria Madentzoglou, Georgios Kravvas and Sandra Jerkovic Gulin
Dermatopathology 2025, 12(2), 10; https://doi.org/10.3390/dermatopathology12020010 - 25 Mar 2025
Abstract
►▼
Show Figures
Dermatofibromas (DFs) represent prevalent benign fibrohistiocytic tumors, typically manifesting as solitary lesions. In the majority of cases, the clinical presentation and dermoscopic and histopathological features of DFs adhere to a characteristic profile. However, DFs may exhibit atypical clinical presentations and, more commonly, histologic
[...] Read more.
Dermatofibromas (DFs) represent prevalent benign fibrohistiocytic tumors, typically manifesting as solitary lesions. In the majority of cases, the clinical presentation and dermoscopic and histopathological features of DFs adhere to a characteristic profile. However, DFs may exhibit atypical clinical presentations and, more commonly, histologic attributes, posing challenges in differential diagnosis. Both DFs and basal cell carcinomas (BCCs) are frequently encountered cutaneous lesions, each characterized by distinct clinical and dermoscopic features and microscopic morphology. The simultaneous occurrence of these two entities within the same lesion is rare. DFs have been documented to form collision tumors in conjunction with a spectrum of benign and malignant lesions, encompassing not only BCC but also balloon cell nevus, squamous cell carcinoma (SCC), and melanoma. Alterations in the epidermis overlaying a DF range from simple hyperplasia to the proliferation of basaloid cells. Accurate diagnosis, leading to the complete excision of the lesion, is contingent upon the recognition of dermoscopic criteria, precluding misinterpretation as a benign lesion. We present two cases of collision tumors comprising DF and BCC. This case report underscores the paramount importance of dermoscopy and adherence to dermoscopic criteria in the assessment of collision lesions and the diagnostic process related to cutaneous malignancies.
Full article
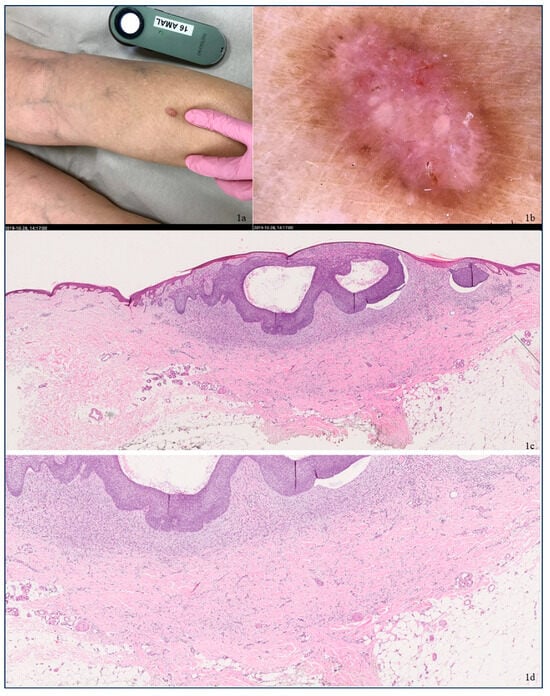
Figure 1
Open AccessReview
Postherpetic Pseudolymphomatous Angiosarcoma Concealed Within Milia en Plaque: Expanding the Spectrum of Wolf Isotopic Response with a Literature Review
by
Marina Corral-Forteza, Noelia Pérez-Muñoz and Maria-Teresa Fernández-Figueras
Dermatopathology 2025, 12(2), 9; https://doi.org/10.3390/dermatopathology12020009 - 22 Mar 2025
Abstract
The Wolf isotopic response (WIR) refers to the development of cutaneous lesions in areas of previously healed but unrelated skin disease. While most are observed in healed herpes zoster, WIR has been reported in various other contexts. Affected areas are believed to exhibit
[...] Read more.
The Wolf isotopic response (WIR) refers to the development of cutaneous lesions in areas of previously healed but unrelated skin disease. While most are observed in healed herpes zoster, WIR has been reported in various other contexts. Affected areas are believed to exhibit immune dysregulation, lymphatic dysfunction, and altered neuromediator activity, increasing susceptibility to inflammatory, neoplastic, and infectious conditions. This phenomenon aligns with the broader concept of the “immunocompromised district”, which also encompasses the Koebner phenomenon and its reverse. Herein, we present the case of a 96-year-old woman who developed multiple cysts and comedones at the site of a resolved herpes zoster. Due to persistent and refractory inflammation, curettage was performed, and histopathological examination revealed angiosarcoma with a pseudolymphomatous reaction interspersed among the cysts. The coexistence of multiple types of WIR is rare but not unprecedented, highlighting the importance of recognizing the diverse pathologic conditions that can arise in such settings. In this review, we explore the historical evolution of terminology used to describe lesions in vulnerable skin areas and related phenomena. We also provide an updated overview of current pathogenic theories and present a comprehensive compilation of postherpetic reactions reported to date.
Full article
(This article belongs to the Section Clinico-Pathological Correlation in Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessReview
Hypertrophic Lichen Planus and Hypertrophic Skin Lesions Associated with Histological Lichenoid Infiltrate: A Case Report and Literature Review
by
Biagio Scotti, Cosimo Misciali, Federico Bardazzi, Bianca Maria Piraccini and Michelangelo La Placa
Dermatopathology 2025, 12(1), 8; https://doi.org/10.3390/dermatopathology12010008 - 25 Feb 2025
Abstract
Hypertrophic lichen planus (HLP) is a chronic inflammatory skin condition defined by verrucous, pruritic, papules and plaques usually affecting the lower limbs. The diagnosis of HLP is primarily clinical. However, due to its feasible generalized presentation and similarities with other hypertrophic cutaneous disorders,
[...] Read more.
Hypertrophic lichen planus (HLP) is a chronic inflammatory skin condition defined by verrucous, pruritic, papules and plaques usually affecting the lower limbs. The diagnosis of HLP is primarily clinical. However, due to its feasible generalized presentation and similarities with other hypertrophic cutaneous disorders, histological evaluation is often necessary. Many dermatological conditions that present with a hypertrophic clinical appearance can arise from a histological lichenoid infiltrate (HCLI). Hence, we provide an overview of the clinical, histopathological, and prognostic features of selected HCLI, including HLP, hypertrophic lichenoid dermatitis, hypertrophic lichen sclerosus (HLS), lichen simplex chronicus (LSC), squamous cell carcinoma (SCC), keratoacanthoma (KA), pseudoepitheliomatous hyperplasia (PEH), viral warts, and lupus erythematosus/lichen planus (LE/LP) overlap. Choosing the appropriate procedure and the anatomical site for an incisional biopsy requires thoughtful consideration to ensure sufficient depth and improve diagnostic accuracy by identifying the histological features specific to each hypertrophic condition.
Full article
(This article belongs to the Section Clinico-Pathological Correlation in Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessReview
Pediatric Kikuchi–Fujimoto Disease: Case Report and Review of Cutaneous and Histopathologic Features in Childhood
by
Alberto Soto-Moreno, Francisco Vílchez-Márquez, María Narváez-Simón, Julia Castro-Martín, Francisco Manuel Ramos-Pleguezuelos, Agustín Soto-Díaz, Jesús Tercedor-Sánchez and Salvador Arias-Santiago
Dermatopathology 2025, 12(1), 7; https://doi.org/10.3390/dermatopathology12010007 - 13 Feb 2025
Abstract
Kikuchi–Fujimoto disease (KFD) is a rare condition characterized by necrotizing lymphadenitis and fever, often associated with immune dysregulation. Histologically, it features necrotic foci with abundant histiocytes and plasmacytoid dendritic cells but notably lacks neutrophils and eosinophils. Recent evidence reveals a notable prevalence among
[...] Read more.
Kikuchi–Fujimoto disease (KFD) is a rare condition characterized by necrotizing lymphadenitis and fever, often associated with immune dysregulation. Histologically, it features necrotic foci with abundant histiocytes and plasmacytoid dendritic cells but notably lacks neutrophils and eosinophils. Recent evidence reveals a notable prevalence among pediatric patients, who may exhibit distinct features compared to adults. We reported the case of an 11-year-old girl presenting with persistent fever, cervical adenopathy, and a malar rash, leading to a diagnosis of KFD following lymph node biopsy, which revealed non-suppurative necrosis and histiocytic infiltration. Empirical treatment with antivirals and antibiotics was ineffective, but corticosteroid therapy achieved symptom remission. A literature review identified 48 relevant studies involving 386 pediatric cases, with histopathological findings consistent with classical descriptions of KFD. Cutaneous involvement was reported in 11.14% of cases, ranging from maculopapular rashes to lupus-like eruptions. Notable complications included the development of systemic lupus erythematous, Sjögren syndrome, and rare instances of hemophagocytic syndrome or central nervous system involvement. Kikuchi–Fujimoto disease should be considered in the differential diagnosis of pediatric patients presenting with fever and lymphadenopathy, taking into account a higher frequency of cutaneous manifestations in pediatric cases. A skin biopsy may be helpful in diagnosing KFD and provide valuable information regarding the potential risk of developing systemic lupus erythematosus in the future.
Full article
(This article belongs to the Section Pediatric Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessSystematic Review
Histologic and Immunohistochemical Patterns in Lymphomatoid Papulosis: A Systematic Review of Published Cases
by
Torben Fricke, Werner Kempf, Michael P. Schön and Christina Mitteldorf
Dermatopathology 2025, 12(1), 6; https://doi.org/10.3390/dermatopathology12010006 - 12 Feb 2025
Abstract
►▼
Show Figures
Based on histologic and genetic patterns, the current World Health Organization (WHO) classification distinguishes six subtypes of lymphomatoid papulosis (Lyp). The aim of our article was to analyze the frequency of histologic and immunohistochemical features of different Lyp subtypes reported in the literature.
[...] Read more.
Based on histologic and genetic patterns, the current World Health Organization (WHO) classification distinguishes six subtypes of lymphomatoid papulosis (Lyp). The aim of our article was to analyze the frequency of histologic and immunohistochemical features of different Lyp subtypes reported in the literature. We used PubMed advanced search builder to systematically review and evaluate English and German literature of Lyp from 1968 to April 2022. We considered only papers in which histopathologic features were mentioned in detail. We identified 48 publications with a total of 518 cases. The diagnoses were based on the diagnostic criteria at the time of publication. In Lyp A and Lyp B a CD8+ phenotype was more often reported than expected (53% and 52%, respectively). A double positive phenotype (CD4+/CD8+) was found in 28% of Lyp E and a double negative (CD4-/CD8-) in 50% of Lyp with 6p25.3 rearrangement. High rates of folliculo- and syringotropism were reported in both Lyp A and B. Surprisingly, strong epidermotropism occurred in 20/38 (53%) cases reported as Lyp B and in 43/64 (67%) of Lyp D cases. The predominating phenotype in Lyp D was CD8+, while TIA-1/granzymeB/perforin expression was reported in 37/46 (80%), and CD56 was expressed in 13/47 (28%) of the investigated cases. The limitation of the data is due to the retrospective approach with diagnostic criteria changing over time and on a case selection in some publications. However, the data indicate that the Lyp subtypes overlap more than assumed. They also show that a prospective study is needed to obtain valid data on the frequency distribution of certain histopathologic criteria.
Full article

Figure 1
Open AccessBrief Report
Acetone–Ether–Water Mouse Model of Persistent Itch Fully Resolves Without Latent Pruritic or Cross-Modality Priming
by
Zachary K. Ford, Adam J. Kirry and Steve Davidson
Dermatopathology 2025, 12(1), 5; https://doi.org/10.3390/dermatopathology12010005 - 11 Feb 2025
Abstract
►▼
Show Figures
Hyperalgesic priming is a model of the transition from acute to chronic pain. Whether a similar mechanism exists for “pruritic priming” of itch is unknown. Here, we tested the hypothesis that itchy skin in a commonly used mouse model of dry skin pruritus
[...] Read more.
Hyperalgesic priming is a model of the transition from acute to chronic pain. Whether a similar mechanism exists for “pruritic priming” of itch is unknown. Here, we tested the hypothesis that itchy skin in a commonly used mouse model of dry skin pruritus develops latent sensitization after resolution. Acetone–ether–water (AEW) treatment induced a dry and itchy skin condition in the mouse cheek that elicited site-directed scratching behavior. After cessation of treatment and the complete resolution of AEW-induced scratching, histaminergic and non-histaminergic pruritogens were administered to the cheek to test for altered site-directed scratching and wiping behavior. Each pruritogen was also tested following the resolution of carrageenan-induced nociceptor hypersensitivity to test for cross-modality priming. Peak AEW-induced scratching occurred 24 h after the final day of treatment, and 5 days were required for scratching levels to return to baseline. Likewise, epidermal thickening was the greatest on the final treatment day and completely returned to baseline after 5 days. After the resolution of itchy cheek skin, acute histamine- and non-histamine-evoked scratching and wiping behaviors were unchanged, nor were scratching and wiping behaviors to acute pruritogens altered after the resolution of carrageenan-induced hypersensitivity. The results indicate that persistent itch due to dry skin likely resolves completely, without producing a latent primed response to subsequent pruritic stimuli. We conclude that the mechanisms regulating hyperalgesic priming are likely distinct from pruritic signaling in the dry and itchy skin model.
Full article

Figure 1
Open AccessCase Report
Asteroid Shower: Cutaneous Silica Granuloma with Asteroid Bodies
by
Fadwa Ahmed and Christopher DiMarco
Dermatopathology 2025, 12(1), 4; https://doi.org/10.3390/dermatopathology12010004 - 31 Jan 2025
Abstract
►▼
Show Figures
Cutaneous silica granulomas are a form of foreign-body granulomatous reactions. They are characterized histopathologically by sarcoidal granulomas in association with silica crystals. Asteroid bodies, a classical histopathological feature of sarcoidosis, have not previously been reported in association with silica granulomas. Herein, we present
[...] Read more.
Cutaneous silica granulomas are a form of foreign-body granulomatous reactions. They are characterized histopathologically by sarcoidal granulomas in association with silica crystals. Asteroid bodies, a classical histopathological feature of sarcoidosis, have not previously been reported in association with silica granulomas. Herein, we present the case of an 83-year-old man with an asymptomatic papule on the vertex scalp. Histopathology revealed a dermal granulomatous reaction to silica crystals. Asteroid bodies were observed in the cytoplasm of multinucleated giant cells. In the absence of systemic symptoms or laboratory findings suggestive of sarcoidosis, a final diagnosis of silica granuloma with asteroid bodies was made. While they have been observed in several other granulomatous reactions, the present case represents a novel association of asteroid bodies with silica granulomas.
Full article

Figure 1
Open AccessReview
Dysplastic Nevi and Superficial Borderline Atypical Melanocytic Lesions: Description of an Algorithmic Clinico-Pathological Classification
by
Sébastien Menzinger, Rastine Merat and Gürkan Kaya
Dermatopathology 2025, 12(1), 3; https://doi.org/10.3390/dermatopathology12010003 - 21 Jan 2025
Abstract
►▼
Show Figures
The diagnosis, interpretation, and classification of melanocytic tumors is a very complex topic in the pathology and dermatopathology field that lacks standardization and is still subject to discordance and debate. Here, we review the definitions of dysplastic nevus and superficial atypical melanocytic proliferations
[...] Read more.
The diagnosis, interpretation, and classification of melanocytic tumors is a very complex topic in the pathology and dermatopathology field that lacks standardization and is still subject to discordance and debate. Here, we review the definitions of dysplastic nevus and superficial atypical melanocytic proliferations and provide an overview of some areas still subject to debate and some attempts of standardization. Furthermore, we describe an algorithmic classification, and provide some examples of clinico-pathological correlation. This step-by-step algorithm has an educational purpose and may automatize the work of dermatopathologists. We hope that through further molecular studies, this fine-grained scheme will prove to be related to the biological behavior of these atypical melanocytic lesions.
Full article

Figure 1
Open AccessClinicopathological Challenge
Violaceous Nodules on the Left Forearm of an Immunosuppressed Patient Following Heart Transplantation for Cardiac Amyloidosis
by
Zachary Corey, Lydia A. Luu, Sabrina Newman and Shyam S. Raghavan
Dermatopathology 2025, 12(1), 2; https://doi.org/10.3390/dermatopathology12010002 - 16 Jan 2025
Abstract
►▼
Show Figures
We present the case of a 60-year-old immunocompromised man who presented with two pruritic pink–red indurated nodules with overlying scale and focal areas of ulceration on his left dorsal and left medial forearm, which evolved over a 2-month period. The pathology showed numerous
[...] Read more.
We present the case of a 60-year-old immunocompromised man who presented with two pruritic pink–red indurated nodules with overlying scale and focal areas of ulceration on his left dorsal and left medial forearm, which evolved over a 2-month period. The pathology showed numerous fungal hyphae present that were pauci-septate with various branched angles and variable hyphal thickness. Fungal cultures grew Rhizopus species and a universal fungal PCR detected the Rhizopus oryzae complex. Based on the clinicopathologic correlation, the diagnosis of cutaneous mucormycosis was made. Cutaneous mucormycosis is an aggressive fungal infection of the Mucorales family occurring after the inoculation of fungal spores in disrupted skin. It usually presents as a necrotic eschar but can also present as cellulitis that evolves into a necrotic ulcer. A prompt diagnosis is critical for the effective management of cutaneous mucormycosis. The treatment includes an immediate systemic treatment with amphotericin B and a surgical debridement of the necrotic regions. Given the wide range of presenting symptoms, clinical suspicion for this emergent condition must remain high in immunocompromised and diabetic patients.
Full article

Figure 1
Open AccessCase Report
Squamomelanocytic Tumor, An Entity Still Shrouded in Mystery: Case Report and Literature Review
by
Joana Sorino, Mario Della Mura, Anna Colagrande, Cecilia Salzillo, Giuseppe Ingravallo and Gerardo Cazzato
Dermatopathology 2025, 12(1), 1; https://doi.org/10.3390/dermatopathology12010001 - 13 Jan 2025
Abstract
►▼
Show Figures
Cutaneous squamomelanocytic tumor (SMT) is a very rare cutaneous malignancy, composed of a dual phenotypic population of both malignant melanocytes and keratinocytes, intimately intermingled together. Herein, we report a new case of a SMT occurring in an 82-year-old man, located on the scalp.
[...] Read more.
Cutaneous squamomelanocytic tumor (SMT) is a very rare cutaneous malignancy, composed of a dual phenotypic population of both malignant melanocytes and keratinocytes, intimately intermingled together. Herein, we report a new case of a SMT occurring in an 82-year-old man, located on the scalp. Histopathology revealed a mixed population consisting of squamous cell carcinoma and melanoma within the same lesion, also confirmed using immunohistochemical staining for high molecular-weight cytokeratins (HMWCKs) and Melan-A. Moreover, to the best of our knowledge, for the first time, we tested SMT for the preferentially expressed antigen in melanoma (PRAME), which revealed a strong and diffuse positivity in the melanocytic component. These tumors need to be distinguished by more frequent collision tumors and colonization. Furthermore, we provide a comprehensive review of the literature, focusing on clinical and histopathological aspects, biological behavior and still-debated, but fascinating histogenesis of this elusive entity.
Full article

Figure 1
Open AccessArticle
Potential Pitfalls of IgG4 Immunohistochemical Staining on Lesional Tissue in Cutaneous Acantholytic Disorders
by
Carla Stephan and Linglei Ma
Dermatopathology 2024, 11(4), 377-382; https://doi.org/10.3390/dermatopathology11040041 - 19 Dec 2024
Abstract
►▼
Show Figures
The diagnostic utility of immunohistochemistry on paraffin-embedded sections in bullous disorders is useful when frozen tissue is not available. In pemphigus vulgaris and pemphigus foliaceus, an intercellular lace-like staining pattern of IgG4 on lesional tissue by immunohistochemistry has been described, with a comparable
[...] Read more.
The diagnostic utility of immunohistochemistry on paraffin-embedded sections in bullous disorders is useful when frozen tissue is not available. In pemphigus vulgaris and pemphigus foliaceus, an intercellular lace-like staining pattern of IgG4 on lesional tissue by immunohistochemistry has been described, with a comparable sensitivity and specificity to direct immunofluorescence on perilesional tissue. This study aimed to evaluate the staining pattern of IgG4 in non-immunobullous disorders to highlight the potential pitfalls when using this stain. In this study, we conducted a retrospective review of our institution’s database of non-immunobullous disorders where immunohistochemistry of IgG4 was performed to rule out pemphigus. We identified 27 cases where IgG4 immunohistochemistry was performed and observed intercellular IgG4 staining in some cases of Grover disease, bullous impetigo, irritated dermal hypersensitivity reaction, acantholytic actinic keratosis, and graft versus host disease. Our results indicate that the interpretation of IgG4 staining by immunohistochemistry in cutaneous acantholytic disorders should be approached with caution. Confirmation on cryosections with direct immunofluorescence study results is important in these settings.
Full article

Figure 1
Open AccessEditorial
New Insights in Paediatric Dermatopathology—2nd Edition
by
Sylvie Fraitag
Dermatopathology 2024, 11(4), 374-376; https://doi.org/10.3390/dermatopathology11040040 - 17 Dec 2024
Abstract
Paediatric dermatology is still an expanding subspeciality, which is well illustrated by the growing number of books and articles that have been published on this subject in recent years [...]
Full article
(This article belongs to the Special Issue New Insights in Paediatric Dermatopathology (2nd Edition))
Open AccessArticle
PRAME Staining of Adnexal Lesions and Common Skin Cancer Types: Biomarker with Potential Diagnostic Utility
by
Hisham F. Bahmad and John Alexis
Dermatopathology 2024, 11(4), 364-373; https://doi.org/10.3390/dermatopathology11040039 (registering DOI) - 12 Dec 2024
Cited by 1
Abstract
PRAME (PReferentially expressed Antigen in MElanoma) is a tumor-associated antigen first identified in tumor-reactive T-cell clones derived from a patient with metastatic melanoma. Immunohistochemistry (IHC) for PRAME is useful for diagnostic purposes to support a suspected diagnosis of melanoma. Anecdotally, PRAME has been
[...] Read more.
PRAME (PReferentially expressed Antigen in MElanoma) is a tumor-associated antigen first identified in tumor-reactive T-cell clones derived from a patient with metastatic melanoma. Immunohistochemistry (IHC) for PRAME is useful for diagnostic purposes to support a suspected diagnosis of melanoma. Anecdotally, PRAME has been observed to stain sebaceous units in glands in background skin. We examined the expression of PRAME in adnexal lesions and common skin cancers to determine whether it is of potential diagnostic utility in supporting the differentiation between sebaceous and non-sebaceous lesions. IRB approval from Mount Sinai Medical Center (MSMC) was obtained. This is a single-center retrospective cohort analysis over a ten-year period (1 January 2012, and 31 December 2023). We used the pathological database of skin lesions, including sebaceous, sweat gland, and follicular lesions, in addition to basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs), from 81 patients who underwent shave/punch biopsies or surgical excisions. We evaluated the IHC staining percentage positivity and intensity for PRAME. Staining intensity was subcategorized into negative, weak, moderate, and strong, whereas expression percentage positivity was subcategorized into 0%, 1–25%, 26–50%, 51–75%, and 76–100%. Most sebaceous versus non-sebaceous lesions exhibited cytoplasmic staining of moderate to strong intensity in >75% of cells. PRAME has a sensitivity and specificity of 100.0% and 86.7%, respectively, to support distinguishing between sebaceous and non-sebaceous adnexal lesions (regardless of whether they are benign or malignant). BCCs and SCCs showed weak to moderate nuclear staining for PRAME in >75% of cells. None of the 13 lesions of hair follicle origin showed any staining. A total of 26 of the 32 lesions of sweat gland origin were negative while 6 (18.75%) showed positive staining. In conclusion, we confirm the potential utility of PRAME for supporting the distinction between sebaceous and non-sebaceous adnexal lesions on one hand, and on the other, distinguishing BCC and SCC that may show nuclear staining from sebaceous carcinoma that shows cytoplasmic staining.
Full article
(This article belongs to the Section Molecular Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessCase Report
A Rare Case of a Malignant Proliferating Trichilemmal Tumor: A Molecular Study Harboring Potential Therapeutic Significance and a Review of Literature
by
Mokhtar H. Abdelhammed, Hanna Siatecka, A. Hafeez Diwan, Christie J. Finch, Angela D. Haskins, David J. Hernandez and Ya Xu
Dermatopathology 2024, 11(4), 354-363; https://doi.org/10.3390/dermatopathology11040038 - 10 Dec 2024
Abstract
►▼
Show Figures
Malignant proliferating trichilemmal tumors (MPTTs), arising from the external root sheath of hair follicles, are exceptionally rare, with limited documentation of their genetic alterations. We present a case of a 64-year-old African American woman who initially presented with a gradually enlarging nodule on
[...] Read more.
Malignant proliferating trichilemmal tumors (MPTTs), arising from the external root sheath of hair follicles, are exceptionally rare, with limited documentation of their genetic alterations. We present a case of a 64-year-old African American woman who initially presented with a gradually enlarging nodule on her posterior scalp. An initial biopsy at an outside hospital suggested metastatic adenocarcinoma or squamous cell carcinoma (SCC) of an uncertain origin. A subsequent wide local excision revealed a 2.0 cm tumor demonstrating characteristic trichilemmal keratinization, characterized by an abrupt transition from the nucleated epithelium to a laminated keratinized layer, confirming MPTT. Immunohistochemistry demonstrated diffuse p53 expression, patchy CD 34 expression, focal HER2 membranous expression, and patchy p16 staining (negative HPV ISH). A molecular analysis identified TP53 mutation and amplifications in the ERBB2 (HER2), BRD4, and TYMS. Additional gene mutations of uncertain significance included HSPH1, ATM, PDCD1 (PD-1), BARD1, MSH3, LRP1B, KMT2C (MLL3), GNA11, and RUNX1. Assessments for the homologous recombination deficiency, PD-L1 expression, gene rearrangement, altered splicing, and DNA mismatch repair gene expression were negative. The confirmation of ERBB2 (HER2) amplification in the MPTT through a molecular analysis suggests potential therapeutic avenues involving anti-HER2 monoclonal antibodies. The presence of the TP53 mutation, without the concurrent gene mutations typically observed in SCC, significantly aided in this differential diagnosis.
Full article

Figure 1
Open AccessCase Report
Digital Papillary Adenocarcinoma Is HPV-42-Associated and BRAFV600E Negative: Perspectives for Diagnostic Practice
by
Tassilo Dege, Arno Rütten, Matthias Goebeler and Hermann Kneitz
Dermatopathology 2024, 11(4), 348-353; https://doi.org/10.3390/dermatopathology11040037 - 9 Dec 2024
Abstract
Digital papillary adenocarcinoma (DPAC) is a rare, low-grade sweat gland carcinoma primarily found on the hands, fingers, or toes and predominantly affecting males. Distinguishing DPAC from benign sweat gland tumors can be challenging. We present the case of a 52-year-old patient with a
[...] Read more.
Digital papillary adenocarcinoma (DPAC) is a rare, low-grade sweat gland carcinoma primarily found on the hands, fingers, or toes and predominantly affecting males. Distinguishing DPAC from benign sweat gland tumors can be challenging. We present the case of a 52-year-old patient with a progressive tumor on the finger initially misdiagnosed as a viral wart. Histological examination revealed a cytologically basophilic sweat gland tumor with tubular structures, papillary protrusions, and a characteristic immunohistochemical staining pattern for CK 7 and Actin. HPV-42 positivity and molecular analysis confirmed the diagnosis of DPAC. HPV-42 has been strongly associated with DPAC. Additionally, p16 positivity and BRAFV600E negativity were observed. These findings aid in the differential diagnosis of acral sweat gland tumors and guide clinical management, including with respect to the potential for recurrence and metastasis.
Full article
(This article belongs to the Section Clinico-Pathological Correlation in Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Atypical Presentation of Spindle Cell Lipoma in a Young Male with a History of Malignant Melanoma
by
Ty Theriot, John David Cattar, Lacey Falgout, Nicholas Culotta and Christopher Haas
Dermatopathology 2024, 11(4), 342-347; https://doi.org/10.3390/dermatopathology11040036 - 26 Nov 2024
Abstract
Spindle cell lipoma (SCL) is a benign adipocytic tumor usually found in the subcutis of the posterior neck, upper back, and shoulder, predominantly in middle-aged males. This case report describes an atypical presentation of SCL in a 26-year-old male with a history of
[...] Read more.
Spindle cell lipoma (SCL) is a benign adipocytic tumor usually found in the subcutis of the posterior neck, upper back, and shoulder, predominantly in middle-aged males. This case report describes an atypical presentation of SCL in a 26-year-old male with a history of malignant melanoma. The patient presented with an erythematous plaque with central hyperpigmentation on the right upper arm, an uncommon location and presentation for SCL. Histopathological examination revealed an atypical myxoid spindle cell neoplasm with CD34 positivity and an overlying mildly atypical compound melanocytic nevus. The unusual clinical and histological features, combined with the patient’s melanoma history, complicated the differential diagnosis, which included dermatofibrosarcoma protuberans (DFSP) and solitary fibrous tumors (SFTs). A wide local excision with 2 cm margins was performed, and subsequent pathology confirmed clear margins, supporting the diagnosis of SCL. This case highlights the importance of including SCL in the differential diagnosis of CD34-positive spindle cell tumors, even when clinical and histological presentations are atypical, and underscores the need for thorough histopathological evaluation and a broad differential diagnosis in patients with a history of melanoma.
Full article
(This article belongs to the Section Clinico-Pathological Correlation in Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessReview
“Chasing Rainbows” Beyond Kaposi Sarcoma’s Dermoscopy: A Mini-Review
by
Emmanouil Karampinis, Olga Toli, Georgia Pappa, Anna Vardiampasi, Melpomeni Theofili, Efterpi Zafiriou, Mattheos Bobos, Aimilios Lallas, Elizabeth Lazaridou, Biswanath Behera and Zoe Apalla
Dermatopathology 2024, 11(4), 333-341; https://doi.org/10.3390/dermatopathology11040035 - 25 Nov 2024
Cited by 1
Abstract
The dermoscopic rainbow pattern (RP), also known as polychromatic pattern, is characterized by a multicolored appearance, resulting from the dispersion of polarized light as it penetrates various tissue components. Its separation into different wavelengths occurs according to the physics principles of scattering, absorption,
[...] Read more.
The dermoscopic rainbow pattern (RP), also known as polychromatic pattern, is characterized by a multicolored appearance, resulting from the dispersion of polarized light as it penetrates various tissue components. Its separation into different wavelengths occurs according to the physics principles of scattering, absorption, and interference of light, creating the optical effect of RP. Even though the RP is regarded as a highly specific dermoscopic indicator of Kaposi’s sarcoma, in the medical literature, it has also been documented as an atypical dermoscopic finding of other non-Kaposi skin entities. We aim to present two distinct cases—a pigmented basal cell carcinoma (pBCC) and an aneurysmatic dermatofibroma—that exhibited RP in dermoscopy and to conduct a thorough review of skin conditions that display RP, revealing any predisposing factors that could increase the likelihood of its occurrence in certain lesions. We identified 33 case reports and large-scale studies with diverse entities characterized by the presence of RP, including skin cancers (Merkel cell carcinoma, BCC, melanoma, etc.), adnexal tumors, special types of nevi (blue, deep penetrating), vascular lesions (acroangiodermatitis, strawberry angioma, angiokeratoma, aneurismatic dermatofibromas, etc.), granulation tissue, hypertrophic scars and fibrous lesions, skin infections (sporotrichosis and cutaneous leishmaniasis), and inflammatory dermatoses (lichen simplex and stasis dermatitis). According to our results, the majority of the lesions exhibiting the RP were located on the extremities. Identified precipitating factors included the nodular shape, lesion composition and vascularization, skin pigmentation, and lesions’ depth and thickness. These parameters lead to increased scattering and interference of light, producing a spectrum of colors that resemble a rainbow.
Full article
(This article belongs to the Special Issue Associations between Dermoscopy and Dermatopathology)
►▼
Show Figures

Figure 1
Open AccessCase Report
A Case of Basal Cell Carcinoma Exacerbated with Akatsuki Disease
by
Yuji Ohara, Issei Kido and Kozo Nakai
Dermatopathology 2024, 11(4), 330-332; https://doi.org/10.3390/dermatopathology11040034 - 22 Nov 2024
Abstract
►▼
Show Figures
Akatsuki disease (also known as pomade crust) is characterized by skin lesions resulting from inadequate skin hygiene. It is sometimes influenced by underlying psychological factors. Akatsuki disease sometimes mimics cutaneous horn or skin cancer. However, there are no previous reports of skin cancer
[...] Read more.
Akatsuki disease (also known as pomade crust) is characterized by skin lesions resulting from inadequate skin hygiene. It is sometimes influenced by underlying psychological factors. Akatsuki disease sometimes mimics cutaneous horn or skin cancer. However, there are no previous reports of skin cancer accompanied with Akatsuki disease. Herein, we report a 79-year-old woman who was referred to our department with a tumor on her left cheek. Before performing a biopsy, we recommended that her family assist with regular facial cleansing. Two months later, the scales and crusts on her entire face had disappeared and the tumor on the left cheek had reduced. Skin biopsy was performed, and histological examination revealed ulcerative basaloid lobules consisting of cells with a small cytoplasm and large hyperchromatic nuclei. Peripheral palisading and tumor-stroma clefting were observed. A diagnosis of basal cell carcinoma was made.
Full article

Figure 1
Open AccessArticle
Image-Guided Radiation Therapy Is Equally Effective for Basal and Squamous Cell Carcinoma
by
Erin M. McClure, Clay J. Cockerell, Stephen Hammond, Evelyn S. Marienberg, Bobby N. Koneru, Jon Ward and Jeffrey B. Stricker
Dermatopathology 2024, 11(4), 315-329; https://doi.org/10.3390/dermatopathology11040033 - 19 Nov 2024
Abstract
►▼
Show Figures
Non-melanoma skin cancers (NMSCs), including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), are highly prevalent and a significant cause of morbidity. Image-guided superficial radiation therapy (IGSRT) uses integrated high-resolution dermal ultrasound to improve lesion visualization, but it is unknown whether efficacy
[...] Read more.
Non-melanoma skin cancers (NMSCs), including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), are highly prevalent and a significant cause of morbidity. Image-guided superficial radiation therapy (IGSRT) uses integrated high-resolution dermal ultrasound to improve lesion visualization, but it is unknown whether efficacy varies by histology. This large retrospective cohort study was conducted to determine the effect of tumor histology on freedom from recurrence in 20,069 biopsy-proven NMSC lesions treated with IGSRT, including 9928 BCCs (49.5%), 5294 SCCs (26.4%), 4648 SCCIS cases (23.2%), and 199 lesions with ≥2 NMSCs (1.0%). Freedom from recurrence at 2, 4, and 6 years was 99.60%, 99.45%, and 99.45% in BCC; 99.58%, 99.49%, and 99.49% in SCC; and 99.96%, 99.80%, and 99.80% in SCCIS. Freedom from recurrence at 2, 4, and 6 years following IGSRT did not differ significantly comparing BCC vs. non-BCC or SCC vs. non-SCC but were slightly lower among SCCIS vs. non-SCCIS (p = 0.002). There were no significant differences in freedom from recurrence when stratifying lesions by histologic subtype. This study demonstrates that there is no significant effect of histology on freedom from recurrence in IGSRT-treated NMSC except in SCCIS. These findings support IGSRT as a first-line therapeutic option for NMSC regardless of histology.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Dermatopathology
Associations between Dermoscopy and Dermatopathology
Guest Editors: Emmanouil Karampinis, Olga ToliDeadline: 30 June 2025